
Background:
Sickle cell crisis is a painful complication of sickle cell disease in adults and children. Acute episodes of severe pain (crises) are the primary reason for hospitalizations. Although infection, dehydration, and acidosis (all of which favor sickling) can act as triggers, in most instances, no predisposing cause is identified. Hospitalizations for sickle cell crisis have been steadily rising over the past decade. Though previous studies have described seasonal variations for in African and Caribbean populations, but there are no large data showing similar trends with patients in the United States. We reviewed a large national hospitalization database to determine whether rates of sickle cell crisis have seasonal variations over the past decade.
Methods:
We examined the Nationwide Inpatient Sample (NIS), a nationally representative survey of hospitalizations conducted by the Healthcare Cost and Utilization Project in collaboration with participating states. It is the largest all-payer inpatient dataset in the United States and includes a 20% sample of United States community hospitals that approximates 20% of all United States community hospitals. The Nationwide Inpatient Sample (NIS) database was used to estimate annual number of hospitalizations from 2000 - 2012. Identification of sickle cell disease related hospitalizations was based on the designation of the prior validated International Classification of Diseases (9th Edition) Clinical Modification (ICD-9-CM) diagnosis code 282.62 (Sickle cell crisis) as the principal discharge diagnosis. The frequency of hospitalization per month cumulative over 13 years was calculated and divided by number of days in that month to determine the mean hospitalizations per day for each month. All calculations were carried out using the weighted estimates approximating nationwide population estimates.
Results:
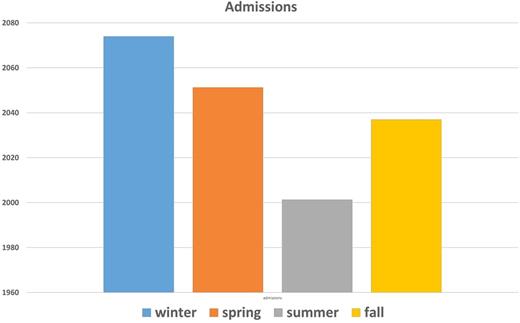
An estimated 744,072 hospitalizations with primary diagnosis of sickle cell crisis occurred in the US from 2000 to 2012. More specifically, the mean number of hospitalizations per day in each month is shown in Fig. 1. The mean number of hospitalizations each day was highest in January (2134 per day) and thereafter the hospitalization rate dropped to a nadir in June (1988 per day). There was a significant rising trend of admissions from June towards winter months with couple of peaks in September and January as depicted in the Fig. 1. In general, the number of hospitalization was maximum in the winter months and minimum in summer months as demonstrated in Fig .2.
Conclusion:
Contrary to expectations, we identified for the first time in United States an impressive pattern of seasonal variation in hospitalizations for sickle cell crisis with a notable increase in winter and fall and a significant drop during summer months. The seasonal pattern may reflect viral or other infections responsible for precipitation of sickle cell crisis. Otherwise, exposure to low temperatures causes increased viscosity of blood and peripheral vasoconstriction triggering sickle cell crisis. This statistical analysis calls for a definitive need to educate patients and providers on how to mitigate the adverse effects of weather on sickle cell crisis. Further efforts need to be done to identify triggers and methods to determine the relationship of these variations and reduce this predictive burden on the overall health care system.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal